There is a lot of talk about insulin resistance in the perimenopause and menopause space. Based on popular messaging, you would think everyone needs to be walking around with continuous glucose monitors and following a “low-carb” diet. But, is that the right approach?
This blog takes a look at what causes insulin resistance, why you are more at risk during perimenopause and menopause for developing insulin resistance, and seven ways you can fight it to help maintain good blood sugar control and overall health.
What Is Insulin Resistance?
Insulin resistance occurs when your muscle, fat, and liver cells become less responsive to insulin, a hormone vital for glucose transport from the bloodstream into your cells to be used for energy.
As a result, blood sugar levels remain elevated, causing the pancreas to produce even more insulin. Over time, this can lead to type 2 diabetes, weight gain, and cardiovascular disease.
Some of the main drivers of insulin resistance are obesity (or excess body fat), a sedentary lifestyle, inflammatory conditions, and a poor diet with excessive calorie, fat, and sugar intake.
This process doesn’t happen overnight. It typically develops gradually over many years.
Increased Risk For Insulin Resistance During Menopause
So, why are you more at risk for insulin resistance during menopause?
Loss of Estrogen
Declining estrogen levels can negatively impact how the body stores fat and uses insulin, making insulin resistance more common. Estrogen plays an important role in maintaining insulin sensitivity.1
Estrogen helps increase the expression and activity of glucose transporters (like GLUT4), especially in muscle and fat cells. This allows cells to take in glucose more efficiently in response to insulin.
Estrogen promotes subcutaneous fat storage and prevents the buildup of visceral fat, which is strongly associated with insulin resistance (more on this next).
Additionally, estrogen helps maintain mitochondrial health and energy metabolism, which plays a role in how cells respond to insulin and manage glucose.
Visceral Fat & Muscle Mass
The decline in estrogen levels during menopause often leads to increased abdominal and visceral fat (abdominal fat surrounding your organs). Visceral fat is metabolically active and secretes inflammatory cytokines (like TNF-α and IL-6) that interfere with insulin signaling pathways, making it harder for cells to respond to insulin.2
Visceral fat releases free fatty acids into the bloodstream, which can accumulate in the liver and muscles. This leads to lipotoxicity, disrupting how insulin works and impairing glucose uptake by cells.
At the same time, you experience a reduction in muscle mass. Women in menopause can lose, on average, about 0.6% of muscle mass each year. 3 Muscle tissue plays a major role in glucose uptake and insulin sensitivity.
Gut Microbiome Changes
Research also suggests that menopause is associated with lower gut microbiome diversity.4 Estrogen plays a role in maintaining a diverse and stable gut microbiome. As estrogen levels decline during menopause, the composition of gut bacteria changes, often leading to a reduction in microbial diversity.
Certain gut bacteria produce compounds (like endotoxins) that can leak into the bloodstream when the gut barrier is compromised, triggering chronic, low-grade inflammation that interferes with insulin signaling in cells.5
Diverse gut bacteria ferment dietary fiber into short-chain fatty acids (SCFAs) like butyrate, which help regulate blood sugar, reduce inflammation, and improve insulin sensitivity. A less diverse microbiome often produces fewer SCFAs, which negatively impacts metabolic regulation.
Movement & Sleep
To compound things, we often become less active during midlife, which can lower insulin sensitivity and contribute to weight gain. Hormonal changes can also impact your sleep quality (hello, insomnia!), and poor sleep is strongly associated with impaired insulin function and metabolic health.
Lack of sleep raises cortisol (the stress hormone), which in turn increases blood sugar levels and promotes fat storage, especially visceral fat, both of which contribute to lower insulin sensitivity.
Sleep deprivation also alters hormones such as leptin (which signals fullness) and ghrelin (which triggers hunger), often leading to increased cravings for sugar and refined carbohydrates, which fuel blood sugar spikes and further strain insulin regulation.
Signs & Symptoms
Insulin resistance often develops silently over time, so it’s important to watch for early signs, especially during menopause.
Here are some common signs and symptoms of insulin resistance:
Physical Signs
- Increased belly fat or difficulty losing weight, especially around the waist
- Frequent fatigue, especially after eating
- Cravings for sugar or carbohydrates
- Dark patches of skin (acanthosis nigricans), often on the neck, armpits, or groin
- Skin tags (small benign growths), especially around the neck or underarms
Metabolic Syptoms
- Elevated fasting blood sugar
- High insulin levels (can be detected with a blood test)
- Elevated triglycerides and/or low HDL (“good”) cholesterol
- High blood pressure
- Brain fog or difficulty concentrating
7 Ways To Fight Insulin Resistance During Menopause
It may sound like your body is setting you up to fail, but the good news is that you can do something about it!
Below are 7 Ways You Can Fight Insulin Resistance During Menopause:
1. Prioritize Sleep

I’m going to start with sleep because it is just that essential, for all the reasons listed above and more. Easier said than done when you’re dealing with insomnia, I know. That’s when you have to really change things up and try “all the things” to see what works best for you.
Below are a few sleep hygiene tips that you have probably heard before but are worth repeating:
- Establish a consistent sleep routine by going to bed and waking up at the same time daily. Your circadian rhythm thanks you!
- Create a cool, dark, quiet sleep environment to support melatonin production and reduce night sweats.
- Limit caffeine and alcohol, especially in the afternoon and evening, as they can interfere with deep sleep.
- Practice relaxation techniques like restorative yoga, meditation, deep breathing, hot baths, sauna, or red light therapy before bed to lower cortisol levels.
- Limit screen time at least an hour before bedtime (this is a tough one for me!). Blue light exposure can disrupt your sleep-wake cycle and reduce melatonin production.
- Avoid late-night eating right before bed. This delays melatonin release and disrupts your quality of sleep, especially deep sleep, where all your cellular repair and recovery take place.
Additionally, I recommend getting some early morning or even midday sun exposure (if that is available to you), which helps regulate melatonin production and synchronize your circadian rhythm. Not only does it signal your body that it’s time to be awake and alert, but it also improves your sleep efficiency at night.
There are sleep tracking devices such as WHOOP and Oura Ring, which can be helpful to see your trends, what impacts or improves your sleep, and how much deep sleep you’re actually getting. I love my Oura Ring for this.
Taking progesterone before bed, in addition to a couple of other helpful supplements, can often be a game-changer. More on this when we discuss HRT and supplements.
2. Choose Quality Carbs
If I had a dollar for every time I’ve heard someone say, “I’m avoiding carbs!” We have demonized carbohydrates so much that they’re now a four-letter word instead of an important macronutrient.
The problem is that carbohydrates are often lumped into one “bad” category without differentiating between refined/processed carbs and healthy complex carbs. The difference lies in their nutrient content, fiber levels, and effect on blood sugar and insulin sensitivity.
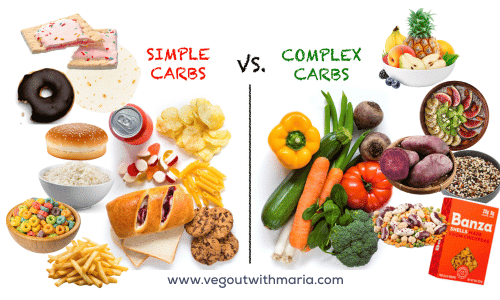
Processed/Refined Carbohydrates
Examples of refined carbs include: white bread, rolls, pastries, sugary cereals, fried noodles, regular pasta, white rice, chips, sweets, sweetened beverages, and most packaged snack foods.
- Highly processed and stripped of fiber, vitamins, and minerals.
- Cause rapid spikes in blood sugar and insulin levels due to fast digestion and absorption.
Frequent consumption of refined carbohydrates can lead to insulin resistance over time, promoting fat gain (especially visceral fat), inflammation, and cravings.
Complex Carbohydrates
On the flip side, there are complex carbohydrates like whole grains (quinoa, oats, farro, wild rice), beans, lentils, sweet potatoes, fruits, and vegetables.
- Digested more slowly, leading to steadier blood sugar and insulin responses.
- Rich in fiber, prebiotics, antioxidants, and nutrients.
- Can help improve insulin sensitivity (particularly those rich in fiber), support gut health, and reduce inflammation, which is especially important during menopause.
While it’s true that complex carbs have less of an impact on blood sugar compared to refined carbs, factors like portion size, overall diet quality, and individual responses can also influence blood sugar levels.
A rise in blood sugar is a natural response to eating, but if you are someone who tracks and notices that you’re seeing a larger spike even when eating small portions of healthy carbs, most likely you are already experiencing insulin resistance.
3. Balance Your Meals With Protein, Fiber, & Healthy Fats

What does it mean to balance your meals?
Balancing your meals means including the right mix of macronutrients (protein, healthy fats, and complex carbohydrates) along with fiber, vitamins, and minerals to support steady energy, hormone balance, and optimal metabolism.
Here’s what a balanced meal typically includes:
- Protein – Helps build and maintain muscle, keeps you full longer, and supports hormone and blood sugar balance.
Examples: Lentils, tofu, tempeh, edamame, beans, quinoa, seitan. - Healthy Fats – Support brain function, hormone production, and absorption of fat-soluble vitamins.
Examples: Avocados, nuts, seeds (like flax, chia, hemp), nut butters, olives. - Complex Carbohydrates – Provide sustained energy and fiber for gut and metabolic health.
Examples: Sweet potatoes, brown rice, oats, legumes, fruits, and vegetables. - Fiber – Slows digestion, improves gut health, and helps regulate blood sugar.
Abundant in plant-based whole foods like veggies, legumes, chia seeds, and whole grains.
Why It Matters
Balanced meals help stabilize blood sugar levels, prevent energy crashes, reduce cravings, and support insulin sensitivity, key for managing weight, mood, and metabolic health.
4. Movement & Exercise

Movement and physical activity are among the most powerful tools for improving insulin resistance! Here’s why:
- Improves Glucose Uptake. Muscles use glucose for fuel during activity. Even light movement (like walking after meals) helps your cells absorb glucose without needing as much insulin, reducing insulin resistance.
- Builds and Maintains Muscle. Muscle is a metabolically active tissue, meaning it helps regulate blood sugar. Strength training and resistance exercises preserve or increase lean muscle mass, which naturally declines with age and menopause.
- Reduces Visceral Fat. Regular exercise, especially strength training, short bursts of high-intensity interval training, and aerobic exercise, helps burn visceral fat (hello, belly fat!), which is strongly linked to insulin resistance, heart disease, diabetes, and certain cancers.
- Lowers Inflammation and Regulates Hormones. Exercise reduces chronic inflammation and improves hormonal balance, both of which are key for maintaining insulin sensitivity.
You don’t need intense workouts. Consistent daily movement is enough to make a big difference. Just 30 minutes a day can enhance insulin function, stabilize blood sugar, and improve overall metabolic health during menopause.
5. Time Restricted Eating
Intermittent fasting is all the rage, but what I personally prefer, and what appears to be a better choice for most women, is time-restricted eating (TRE).
Time-restricted eating (TRE) is a form of intermittent fasting that focuses on eating within a consistent daily window (usually 8–12 hours) and fasting for the remaining hours, typically overnight.
While both TRE and broader intermittent fasting approaches can be helpful, TRE may be especially beneficial and sustainable for menopausal women, particularly when it comes to improving insulin resistance.

How TRE Differs From General Intermittent Fasting:
Intermittent fasting often includes longer fasts (like 16:8, 24-hour fasts, or alternate-day fasting), which may be too stressful for women in menopause, potentially worsening cortisol levels and hormone balance.
Time-restricted eating encourages a daily rhythm that’s aligned with your circadian biology, making it easier on the body and more adaptable long term.
Why TRE is Especially Beneficial for Menopausal Women:
1. Supports Circadian Rhythms: Eating earlier in the day and fasting overnight aligns with the body’s natural clock, improving metabolic efficiency and hormone regulation, both of which can be disrupted during menopause.
2. Improves Insulin Sensitivity: TRE gives the body longer breaks from food, reducing frequent insulin spikes. Over time, this helps lower fasting insulin levels, improve glucose control, and reduce the risk of type 2 diabetes.
3. Reduces Visceral Fat and Inflammation: Shortening the eating window helps regulate energy intake and fat metabolism, especially abdominal fat, which is strongly linked to insulin resistance and increases after menopause.
4. Enhances Cellular Repair: Fasting periods activate processes like autophagy (cellular cleanup), which can improve metabolic health, reduce oxidative stress, and support healthy aging.
It’s as simple as starting with a 12-hour window (e.g., 7am–7pm), which is pretty easy to do since a majority of that time is spent sleeping. You can gradually work toward shortening your eating window to find what works best for you and your body. There is no ideal time for everyone.
Prioritize protein and fiber-rich meals earlier in the day to stabilize blood sugar and energy, and avoid late-night eating, as insulin sensitivity naturally declines in the evening. When you pair TRE along with strength training, you help prevent sarcopenia (muscle wasting).6
6. Stress Management
It’s easy to underestimate the power stress has on your body, but managing stress is crucial for improving insulin sensitivity, especially during menopause when hormonal shifts already challenge blood sugar control.
Chronic stress raises cortisol, a hormone that increases blood glucose and promotes insulin resistance and abdominal fat storage.
Activating the parasympathetic nervous system, your body’s “rest and digest” mode, helps counteract stress by lowering cortisol levels, calming inflammation, and improving how your cells respond to insulin. Practices like deep breathing, meditation, yoga, walking in nature, and mindful eating can support this relaxation response, enhancing both metabolic health and hormonal balance.

For my stress management practice, I choose to meditate for 5-15 minutes first thing in the morning before exercise. This helps me set the tone for my day and better equip me to handle some of the daytime stressors. I also enjoy winding down my day with some herbal adaptogen tea and an occasional relaxing bath before bed.
Find a stress management tool that works for you and implement this practice daily for best results.
7. HRT & Supplements
Hormone replacement therapy (HRT), particularly estrogen therapy, can improve insulin sensitivity in menopausal women by addressing the metabolic effects of estrogen loss as described earlier.7 I can tell you personally that it was a game-changer for me!
In perimenopause, when estrogen often dominates over low progesterone (“estrogen dominance”) because of declining progesterone levels, restoring progesterone can help rebalance hormones, potentially easing weight gain and blood sugar fluctuations.
Progesterone also has calming, sleep-promoting effects, which can lower cortisol levels. Since poor sleep and chronic stress worsen insulin resistance, better rest can indirectly support metabolic health.
The potential benefits of HRT go far beyond improving insulin response. HRT can be an effective treatment for hot flashes and night sweats, help support cognitive and mood health, improve sleep quality, protect your bones, and have cardiovascular benefits.
Ultimately, it is your decision if HRT is right for you. Unfortunately, most doctors – even OBGYN specialists – have very little up-to-date knowledge on this topic. I encourage you to find a doctor who specializes in HRT so you can be given all the facts to make an informed decision.
What About Supplements?
Several supplements have shown promise in improving insulin sensitivity and managing insulin resistance, including omega-3 fatty acids, magnesium, chromium, berberine, cinnamon, vitamin D, inositol, and probiotics.
The role of creatine for muscle and metabolic health has also been shown to be beneficial (for more on creatine, I recommend reading Creatine For Menopause).
While these supplements may have some benefit (especially omega-3, magnesium, and vitamin D), they are only part of a broader strategy that includes dietary changes, sleep quality, exercise, and stress management.
Bottomline
Insulin resistance is a major health concern during menopause, driven by hormonal shifts that affect metabolism, fat distribution, and blood sugar control. Left unaddressed, it can have a profound impact on your overall health.
However, this doesn’t mean we all need to be walking around with continuous glucose monitors (CGMs). At this point, there’s not a lot of published evidence showing that monitoring glucose levels is beneficial or even accurate for those without diabetes, and why would we want to add more unnecessary stress and anxiety around eating?
To me, it seems counterproductive in a time when we should be focusing on releasing stress and developing a healthier relationship with our food.
The good news? You do have the power to shift things and improve your insulin sensitivity. Small, consistent lifestyle changes, like prioritizing sleep, staying active, managing stress, and embracing a balanced, plant-based (or at least plant-forward) diet, can make a powerful difference.
Other Articles To Explore…